The medical system itself is a major barrier to management of obesity. Numerous studies find that clinicians, including medical trainees and nurses, harbor negative stereotypes toward patients with overweight/obesity, and that they often feel a sense of pessimism about the eventual success of their weight-loss counseling and obesity management efforts.9-14 These negative attitudes are apparent to patients and can negatively influence patient receptiveness to weight-loss counseling messages.15, 16 It can also prevent patients from seeing their clinician for non obesity-related health issues.29
In part, clinicians’ pessimism may originate from unrealistic standards for what constitutes “success” in a weight loss program. Too often the focus is on reaching an ideal body weight, which is often unrealistic and discourages compliance with the prescribed program of diet and exercise.30
Physicians may also feel obligated to advise an “all-or-none” strategy to their patients, which carries a high risk of failure. The reality is that even modest weight loss (10% of body weight) has been shown to markedly improve blood pressure, serum cholesterol, and glucose tolerance.30, 31
At the same time, how physicians frame weight-loss messages with their patients is important. For instance, patients are more receptive to positive (“gain-framed”), motivational discussions focusing on the health benefits of moderate weight loss, than to negative (“loss-framed”) discussions of the risks of remaining overweight. Similarly, positively framed messages are perceived as more effective in promoting exercise than negatively framed messages.32-34
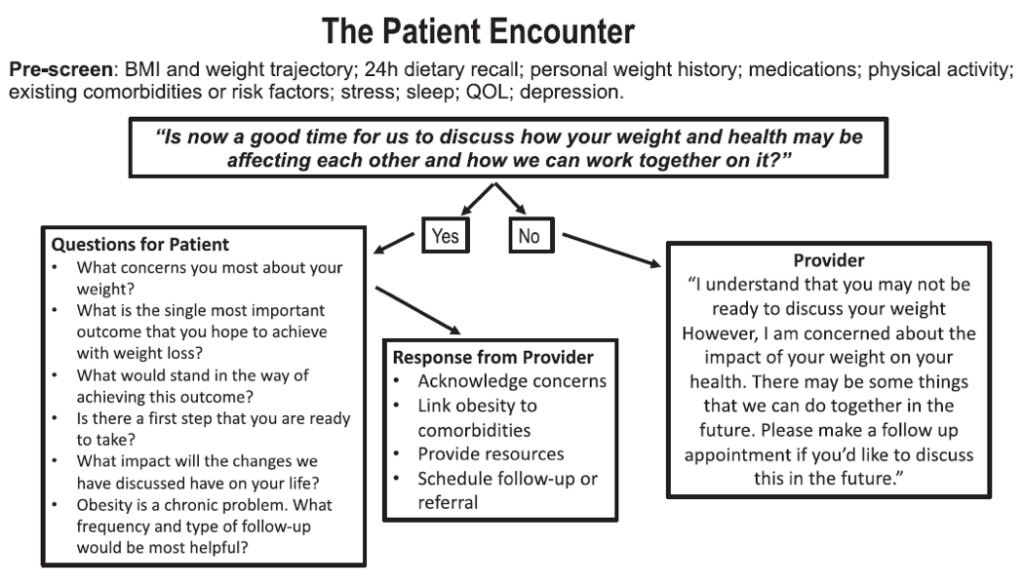
Other communication strategies have been formally studied for their effectiveness in motivating patients to take control of their weight problems. For instance, the “5As counseling technique” (Assess risk, current behavior, and readiness to change; Advise change of specific behaviors; Agree and collaboratively set goals; Assist in addressing barriers and securing support; and Arrange for follow up) is associated with better outcomes when used to counsel obesity patients.35
Finally, clinicians should use shared decision making when discussion weight loss/management options with their patients. This involves both the clinician and the patient working together to come up with a treatment decision based on their knowledge of the options and of the patient’s personal preferences and values.36