Talking to Patients About Obesity
The medical system itself is a major barrier to management of obesity. Numerous studies find that clinicians, including medical trainees and nurses, harbor negative stereotypes toward patients with overweight/obesity, and that they often feel a sense of pessimism about the eventual success of their weight-loss counseling and obesity management efforts.9-14 These negative attitudes are apparent to patients and can negatively influence patient receptiveness to weight-loss counseling messages.15, 16 It can also prevent patients from seeing their clinician for non obesity-related health issues.29
In part, clinicians’ pessimism may originate from unrealistic standards for what constitutes “success” in a weight loss program. Too often the focus is on reaching an ideal body weight, which is often unrealistic and discourages compliance with the prescribed program of diet and exercise.30
Physicians may also feel obligated to advise an “all-or-none” strategy to their patients, which carries a high risk of failure. The reality is that even modest weight loss (10% of body weight) has been shown to markedly improve blood pressure, serum cholesterol, and glucose tolerance.30, 31
At the same time, how physicians frame weight-loss messages with their patients is important. For instance, patients are more receptive to positive (“gain-framed”), motivational discussions focusing on the health benefits of moderate weight loss, than to negative (“loss-framed”) discussions of the risks of remaining overweight. Similarly, positively framed messages are perceived as more effective in promoting exercise than negatively framed messages.32-34
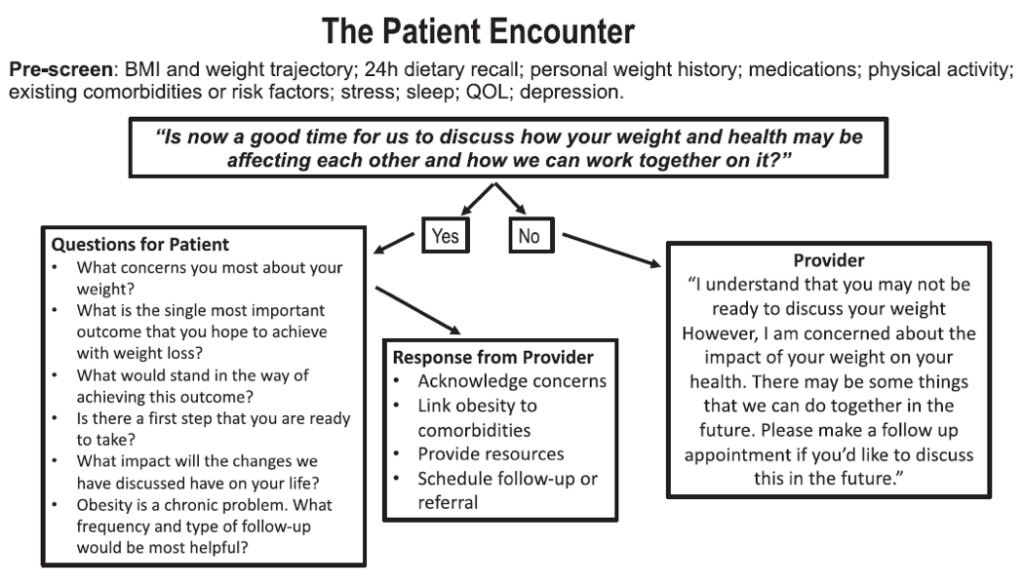
Other communication strategies have been formally studied for their effectiveness in motivating patients to take control of their weight problems. For instance, the “5As counseling technique” (Assess risk, current behavior, and readiness to change; Advise change of specific behaviors; Agree and collaboratively set goals; Assist in addressing barriers and securing support; and Arrange for follow up) is associated with better outcomes when used to counsel obesity patients.35
Finally, clinicians should use shared decision making when discussion weight loss/management options with their patients. This involves both the clinician and the patient working together to come up with a treatment decision based on their knowledge of the options and of the patient’s personal preferences and values.36
References
- Centers for Disease Control and Prevention. Adult Obesity Facts. Accessed June 26, 2023, https://www.cdc.gov/obesity/data/adult.html
- Abdel-Malek M, Yang L, Miras AD. Pharmacotherapy for chronic obesity management: a look into the future. Intern Emerg Med. 2023;doi:10.1007/s11739-023-03237-4
- Marx J. Cellular warriors at the battle of the bulge. Science. 2003;299(5608):846-9. doi:10.1126/science.299.5608.846
- Authesserre N, et al. Cell Biology Promotion. Accessed June 27, 2023, www.cellbiol.net/ste/alpobesity2.php
- Berg S. AMA: Use of BMI alone is an imperfect clinical measure. Accessed June 25, 2023, https://www.ama-assn.org/delivering-care/public-health/ama-use-bmi-alone-imperfect-clinical-measure
- Centers for Disease Control and Prevention. Defining adult overweight & obesity. Accessed June 27, 2023, www.cdc.gov/obesity/adult/defining.html
- Stanford FC, Lee M, Hur C. Race, Ethnicity, Sex, and Obesity: Is It Time to Personalize the Scale? Mayo Clin Proc. 2019;94(2):362-363. doi:10.1016/j.mayocp.2018.10.014
- Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society. J Am Coll Cardiol. 2014;63(25 pt B):2985-3023. Not in File. doi:S0735-1097(13)06030-0;10.1016/j.jacc.2013.11.004
- Garvey WT, Mechanick JI, Brett EM, et al. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22 Suppl 3:1-203.
- Apovian CM, Garvey WT, Ryan DH. Challenging obesity: Patient, provider, and expert perspectives on the roles of available and emerging nonsurgical therapies. Obesity (Silver Spring). 2015;23 Suppl 2(0 2):S1-s26. doi:10.1002/oby.21140
- Idrees Z, Cancarevic I, Huang L. FDA-Approved Pharmacotherapy for Weight Loss Over the Last Decade. Cureus. 2022;14(9):e29262. doi:10.7759/cureus.29262
- Drugs.com. Phendimetrazine Tablets Prescribing Information. Accessed June 26, 2023, https://www.drugs.com/pro/phendimetrazine-tablets.html
- Drugs.com. Benzphetamine Prescribing Information. Accessed June 26, 2023, https://www.drugs.com/pro/benzphetamine.html
- Stanford FC, Alfaris N, Gomez G, et al. The utility of weight loss medications after bariatric surgery for weight regain or inadequate weight loss: A multi-center study. Surg Obes Relat Dis. 2017;13(3):491-500.
- SAXENDA (liraglutide) injection for subcutaneous use [prescribing information]. Plainsboro NNNI.
- WEGOVY (semaglutide) injection, for subcutaneous use [prescribing information]. Plainsboro, NJ: Novo Nordisk Inc; 2021.
- Kadouh H, Chedid V, Halawi H, et al. GLP-1 Analog Modulates Appetite, Taste Preference, Gut Hormones, and Regional Body Fat Stores in Adults with Obesity. J Clin Endocrinol Metab.
- Wilding JPH, Batterham RL, Calanna S, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021;384(11):989-1002. doi:10.1056/NEJMoa2032183
- Wilding JPH, Batterham RL, Calanna S, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021;384(11):989-1002. doi:10.1056/NEJMoa2032183
- Mehta A, Marso SP, Neeland IJ. Liraglutide for weight management: a critical review of the evidence. Obes Sci Pract. 2017;3(1):3-14. doi:10.1002/osp4.84
- Holst JJ. Incretin-based therapy of metabolic disease. Dan Med J. 2022;70(1)
- Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med. 2022;387(3):205-216. doi:10.1056/NEJMoa2206038
- Rosenstock J, Wysham C, Frías JP, et al. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet. 2021;398(10295):143-155. doi:10.1016/s0140-6736(21)01324-6
- Ludvik B, Giorgino F, Jódar E, et al. Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet. 2021;398(10300):583-598. doi:10.1016/s0140-6736(21)01443-4
- Eisenberg D, Shikora SA, Aarts E, et al. 2022 American Society for Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO): Indications for Metabolic and Bariatric Surgery. Surg Obes Relat Dis. 2022;18(12):1345-1356. doi:10.1016/j.soard.2022.08.013
- Balasubaramaniam V, Pouwels S. Remission of Type 2 Diabetes Mellitus (T2DM) after Sleeve Gastrectomy (SG), One-Anastomosis Gastric Bypass (OAGB), and Roux-en-Y Gastric Bypass (RYGB): A Systematic Review. Medicina (Kaunas). 2023;59(5)doi:10.3390/medicina59050985
- Chandrakumar H, Khatun N, Gupta T, Graham-Hill S, Zhyvotovska A, McFarlane SI. The Effects of Bariatric Surgery on Cardiovascular Outcomes and Cardiovascular Mortality: A Systematic Review and Meta-Analysis. Cureus. 2023;15(2):e34723. doi:10.7759/cureus.34723
- O’Brien PE, Hindle A, Brennan L, et al. Long-Term Outcomes After Bariatric Surgery: a Systematic Review and Meta-analysis of Weight Loss at 10 or More Years for All Bariatric Procedures and a Single-Centre Review of 20-Year Outcomes After Adjustable Gastric Banding. Obes Surg. 2019;29(1):3-14. doi:10.1007/s11695-018-3525-0
- Alberga AS, Edache IY, Forhan M, Russell-Mayhew S. Weight bias and health care utilization: A scoping review. Prim Health Care Res Dev. 2019;20:e116. doi:10.1017/s1463423619000227
- Alpert JS. “So, doctor, what’s so bad about being fat?” Combating the obesity epidemic in the United States. Am J Med. 2010;123:1-2. doi:10.1016/j.amjmed.2009.05.027
- Magkos F, Fraterrigo G, Yoshino J, et al. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 2016;23:591-601. doi:10.1016/j.cmet.2016.02.005
- Bartels RD, Kelly KM, Rothman AJ. Moving beyond the function of the health behaviour: The effect of message frame on behavioural decision-making. Psychol Health. 2010;25:821-838. doi:10.1080/08870440902893708
- Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: The role of message framing. Psychol Bull. 1997;121:3-19. doi:10.1037/0033-2909.121.1.3
- Campbell MK, DeVellis BM, Strecher VJ, Ammerman AS, DeVellis RF, Sandler RS. Improving dietary behavior: The effectiveness of tailored messages in primary care settings. Am J Public Health. 1994;84:783-787. doi:10.2105/ajph.84.5.783
- Jay M, Gillespie C, Schlair S, Sherman S, Kalet A. Physicians’ use of the 5As in counseling obese patients: Is the quality of counseling associated with patients’ motivation and intention to lose weight? BMC Health Serv Res. 2010;10:159. doi:10.1186/1472-6963-10-159
- Sarwer DB, Gasoyan H, Bauerle Bass S, Spitzer JC, Soans R, Rubin DJ. Role of weight bias and patient- physician communication in the underutilization of bariatric surgery. Surg Obes Relat Dis. 2021;17:1926-1932. doi:10.1016/j.soard.2021.07.013
Gallagher C, Corl A, Dietz WH. Weight can’t wait: A guide to discussing obesity and organizing treatment in the primary care setting. Obesity (Silver Spring). 2021;29:821–824. doi:10.1002/oby.23154